What happens to cancer cells after they're killed by treatments?
Cancer treatments aim to kill tumor cells, and the immune system is tasked with getting rid of the resulting corpses.
Cancer treatments like chemotherapy kill tumor cells, for example, by pushing them to self-destruct, shrivel up and quietly die in a process called apoptosis, or less commonly, by triggering a more explosive form of cell death called necroptosis.
But what happens to those cancer cells after they've been slain?
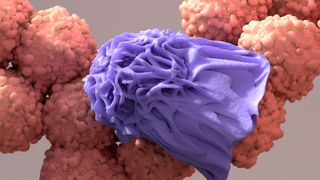
When cancer cells meet their demise, their membranes usually become compromised, as occurs in apoptosis, a form of programmed cell death that removes unneeded or damaged cells from the body. Once the molecular switches that trigger apoptosis are flipped "on," the dying cell shrinks and bits of its membrane break away in "blebs." This causes the cells' internal components to leak out and attract phagocytes, or immune cells responsible for ingesting cellular debris.
The summoned phagocytes engulf the dead cancer cells and then break them down into smaller components, such as sugars and nucleic acids, chain-like molecules found in DNA. Via this process, dead cancer cells are recycled into components that can be reused by other cells.
Related: Does it matter what time of day you get cancer treatment?
In the case of apoptosis — the type of cell death cancer therapies are traditionally designed to induce — cellular components are generally recycled in this way rather than excreted by the body. Cancer therapies can sometimes also trigger other types of cell death, like necroptosis, in which cells swell and burst rather than shrinking, and phagocytes also efficiently gobble up this type of dying cell.
However, dying cancer cells don't always go quietly. Studies suggest that, by releasing debris that sparks inflammation, dying cancer cells can sometimes stimulate the growth of surviving cancer cells.
This phenomenon, known as the Révész effect, may help explain how some cancers come back after treatment. It was first observed in the 1950s in mice with tumors. More recently, a 2018 study in mice and cells in lab dishes found that radiation and chemotherapy can trigger the release of proinflammatory cytokines, molecules released by immune cells that drive up inflammation that can sometimes support tumor growth.
Macrophages, a type of phagocyte, release these molecules in an attempt to fight the cancer, Dr. Dipak Panigrahy, a study co-author and assistant professor of pathology at Beth Israel Deaconess Medical Center in Boston told Live Science.
A 2023 study conducted by a different group found that the nuclei of dying cancer cells can sometimes swell and burst, releasing DNA and other molecules into their surroundings. In mice, these spilled molecules can accelerate metastasis, the spread of cancer cells beyond their original tumor.
These studies help to shed light on the role of tumor cell death on cancer progression and relapse — however, research is still in relatively early stages and scientists don't yet to understand the full implications of dying cancer cell signaling in human cancer. With more research, researchers aim tol better understand the biological mechanisms underlying cancer and thereby develop more effective treatments.
For example, the 2018 study highlighted a way to counter the tumor growth driven by dead cancer cell debris: resolvins, molecules derived from omega 3 that can help reduce inflammation and the effects of cytokines while prompting the clearance of cell debris.
"The problem in cancer is that there are no therapies that stimulate the resolution of inflammation and down-regulate cytokines and clear debris," Panigrahy said. Resolvins could be one way of addressing those problems, their study suggests.
In addition, the 2023 Nature study pinpointed how living cancer cells recognize and respond to the signals transmitted by their dying peers. Blocking the dying cells' messages could help prevent cancer from re-emerging after treatment, the study hints.
This article is for informational purposes only and is not meant to offer medical advice.
Live Science newsletter
Stay up to date on the latest science news by signing up for our Essentials newsletter.
Sarah Moore is a freelance science writer. She has an MSc in neuroscience and a BSc in psychology from Goldsmiths College, University of London. Sarah has experience in academic research and has worked in medical communications with top pharmaceutical companies. As a freelancer, she has contributed work to a wide range of publications. Sarah loves to write on all areas of science, from healthcare to nanotechnology but she is especially intrigued by the workings of the human brain.
-
Homer10 This is like the problem created by Meningitis. If the bacteria is allowed to go too far, When an antibiotic is given, the problems can get worse because all those bacteria are now being exploded from the inside by the antibiotic, and the pieces of the bacteria that are left over still can cause havoc. So in this case an antibiotic can actually help in causing the demise of the patient. Anti-Inflamitories have been found to help with this situation.Reply

